Clogging the flow: Impaired glymphatic function as a hallmark of neuroinflammation
The glymphatic system is responsible for clearing toxic metabolites from the brain during sleep. This network of perivascular spaces lined by astrocytic end feet enables the bulk fluid movement of cerebrospinal fluid into, and interstitial fluid through the brain. Decreased glymphatic function, and thus decreased clearance of waste, has been associated with age, Alzheimer’s disease, diabetes, hypertension, traumatic brain injury, chronic high ethanol intake, chronic unpredictable stress, bacterial meningitis, and, preliminarily, pain.
The majority of these conditions that exhibit glymphatic dysfunction are also associated with increased neuroinflammation characterized in part by increased inflammatory cytokines and reactive gliosis. The main goal of this master’s proposal is to understand how neuroinflammation may alter the structure of the glymphatic system, either in the perivascular or interstitial space, leading to a reduction in flow. This project will involve a combination of live-animal surgery, ex vivo and in vivo imaging, in vivo microdialysis, immunohistochemistry and more.
This project has a special emphasis on chronic pain, a debilitating condition with no effective, non-addictive treatment. We use two pre-clinical models of chronic neuropathic pain: sparse nerve injury and spinal chord injury. Our goal is to understand glymphatic dysfunction in chronic pain, and potentially develop therapeutics to increase glymphatic flow after development of neuroinflammatory pathology.
The project will take place in the Center for Translational Neuromedicine (CTN) at the University of Copenhagen and the University of Rochester Medical Center. CTN is an international research group of more than 50 people, with collaborations that span the globe, providing exposure to a wide array of scientific questions centered around glial cells. CTN features state-of-the-art facilities and equipment, joint weekly journal clubs and focus groups between Copenhagen and Rochester, and integrative training among undergraduates, graduate students, postdocs and faculty. By integrating international teams and training levels, trainees are exposed to all levels of science from benchwork to science writing to project development.
This project is a collaboration between Dr. Lauren Hablitz, an expert in glymphatic function, and Dr. Maiken Nedergaard, an expert in glial biology, pain, and discoverer of the glymphatic system. As such, this project will involve research done in Rochester, New York, USA. The lab language is English, and international as well as Danish students are welcome.
Please send your application including a short CV and a short letter of motivation to Dr. Hablitz or Dr. Nedergaard.
Lauren Hablitz, PhD
Assistant Professor
Department of Neurology
Center for Translational Neuromedicine
University of Rochester Medical Center
lauren_hablitz@urmc.rochester.edu
https://www.urmc.rochester.edu/labs/hablitz.aspx
Maiken Nedergaard, MD, DMSc
Professor
Center for Translational Neuromedicine
University of Copenhagen
https://ctn.ku.dk/research/nedergaard_laboratory/
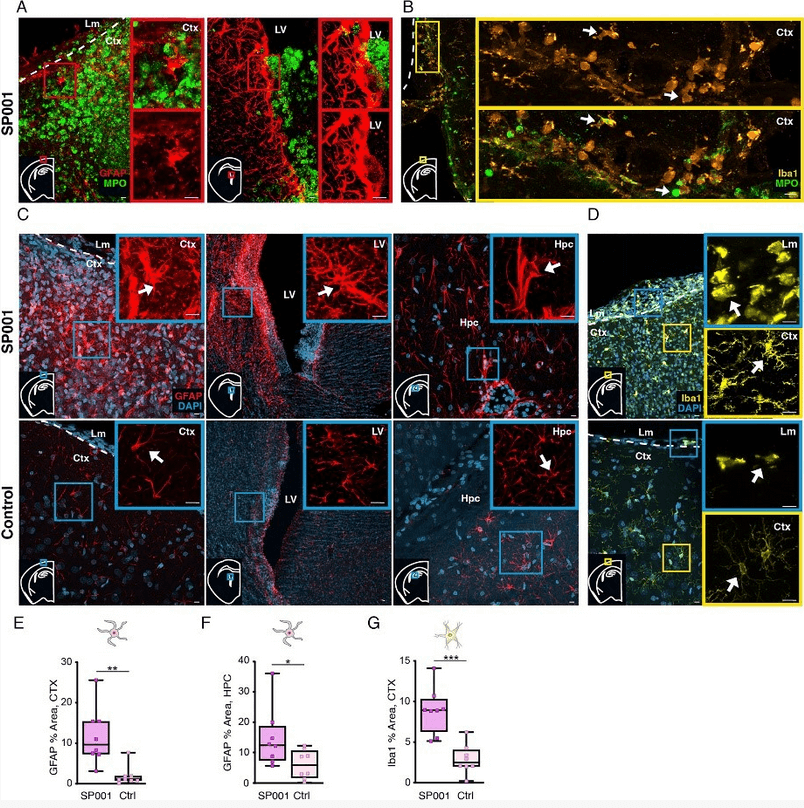
Streptococcus pneumoniae meningeal infection promotes gliosis in the brain parenchyma. (A–D) Confocal microscopy of coronal brain sections obtained from S pneumoniae–infected (A, C, upper panel) and control rat brains immunolabeled for glial fibrillary acidic protein (GFAP; A, C; red), microglial/macrophage ionized calcium‐binding adapter molecule 1 (Iba1; B, D; yellow), and neutrophil myeloperoxidase (MPO; A; green) and counterstained with 4',6‐diamidino‐2‐phenylindole (DAPI; blue). (A,C) In infected animals, astrogliosis was observed in brain areas with bacterial proliferation and recruitment of neutrophils such as the meninges and the lateral ventricle (LV), and also in areas where bacteria and neutrophils were not detected, namely the hippocampus (Hpc; C, arrow). (A) Direct cell–cell contacts between astrocytes and neutrophils were observed in the meninges and in the lateral ventricle. (C, lower panel) Astrocytes were not activated in the meninges, lateral ventricle, and hippocampus of control animals. Activated and hypertrophic microglia were observed in the meninges of infected rats (B, D, yellow inset, arrows), in direct contact with infiltrating neutrophils. There was also a massive presence of meningeal macrophages (B, D, blue inset, arrows), directly interacting with neutrophils (B, arrows). In sharp contrast, there was no sign of microglial activation in control animals (D, lower panel, arrows), which had only sporadic macrophages present in the meninges. (E–G) Quantification of GFAP immunoreactivity in the cortex (CTX; E) and hippocampus (F) and Iba1+ immunoreactivity in the cortex (G; unpaired t‐test with Holm–Šídák multiple comparison adjustment, *p < 0.05,
**p < 0.01, ***p < 0.001). Error bars represent ± standard deviation, n = 8 in each group. Scale bars: 10μm. Lm = leptomeninges; SP001 = S pneumoniae strain 001. Annals of Neurology, Volume: 90, Issue: 4, Pages: 653-669, First published: 16 August 2021, DOI: (10.1002/ana.26186).
